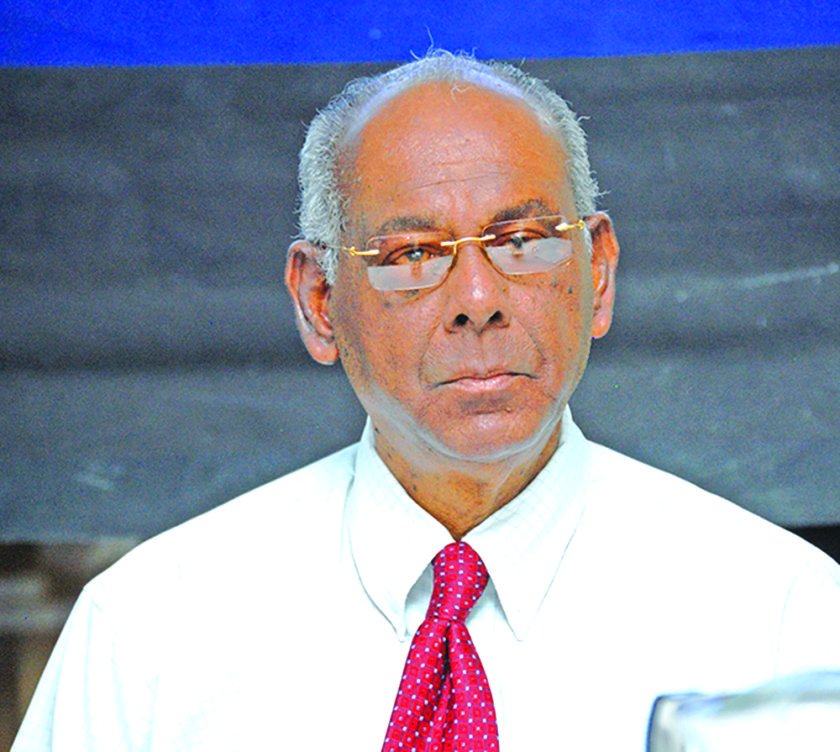
Mental Health Unit Director, Dr Util Richmond-Thomas said that owing to the alarming number of self-harm cases, the decision has been taken to launch “The National Self-Harm Surveillance” project come July.
“If we can get the majority of self-harm and depression cases treated, we can drastically reduce the suicide rate,” the Director was quoted as saying in an interview with the Government Information Agency (GINA).
Self-harming cases are also known as non-suicidal self-injury. Dr Richmond-Thomas explained that in Region Three (West Demerara-Essequibo Islands) alone, 93 self-harm cases have already been recorded for 2017. Thirty suicide deaths were officially recorded at the West Demerara Regional Hospital for the same period. The National Self- Harm Surveillance project will be launched initially in Regions Two, Three and Six, mainly because those regions have the highest suicide rates.
“Self-harm is the strongest indicator of future suicide,” Dr Richmond-Thomas stated. According to the GINA release, she further explained that many persons who commit suicide would have had several incidents of self-harm in their past. “It means, therefore, that if the self-harm was being treated while it was occurring, it may not have led to suicide.”
The Programme Director, in explaining how the project would work, said all cases of self-harm must be reported to the Mental Health Unit within one week of presentation. Once reported, persons will then have to see a psychiatrist or mhGAP (mental health GAP-IG) doctor. There are over 40 mhGAP doctors locally. Each case will receive psychotherapy by a psychologist and be followed up by a social worker until they are no longer high-risk patients.
The Unit will also be implementing a self-harm screening tool, which is a questionnaire. The questionnaire will aid in the fight against suicide. The pilot screening tool is expected to be rolled out in three major hospitals in Regions Two, Three and Six soon.
“Making sure they (patients) are properly treated will just ensure that they have better quality of life,” Dr Richmond-Thomas added. She said the Unit’s drive to battle suicide was “well on its way”, with the Public Health Ministry rolling out several mental health projects.
“The National Self-Harm Surveillance follows closely on the heels of the mhGAP Intervention Guide programme, which recently saw non-specialised doctors trained with the necessary skills and knowledge to better screen patients and provide diagnostic assessment for persons living with mental health illnesses. This programme seeks to provide efficient care at primary health-care facilities across the nation. This programme is part Guyana’s National Mental Health Action Plan 2015-2020.