 Cervical cancer is the fourth most frequent cancer in women with an estimated 570,000 new cases in 2018 representing 6.6% of all female cancers. Approximately 90% of deaths from cervical cancer occurred in low- and middle-income countries.
Cervical cancer is the fourth most frequent cancer in women with an estimated 570,000 new cases in 2018 representing 6.6% of all female cancers. Approximately 90% of deaths from cervical cancer occurred in low- and middle-income countries.
The high mortality rate from cervical cancer globally could be reduced through a comprehensive approach that includes prevention, early diagnosis, effective screening and treatment programmes. There are currently vaccines that protect against common cancer-causing types of human papilloma virus and can significantly reduce the risk of cervical cancer.
Early diagnosis
Particularly in countries where screening programmes are not available, diagnosing cervical cancer at an early stage and providing access to effective treatment can significantly improve the likelihood of survival. Currently, in many low resource settings, the disease is often not identified until it is further advanced or treatment is inaccessible resulting in a higher rate of death from cervical cancer. Understanding and detecting symptoms of cervical cancer can assist with early diagnosis.
Symptoms of cervical cancer tend may include: irregular, intermenstrual (between periods) or abnormal vaginal bleeding after sexual intercourse; back, leg or pelvic pain; fatigue, weight loss, loss of appetite; vaginal discomfort or odourous discharge; and a single swollen leg. More severe symptoms may arise at advanced stages. WHO Package of essential noncommunicable (PEN) disease interventions for primary health care in low-resource settings has guidance on the approach to assessment and referral for women with suspected cervical cancer in the primary care setting.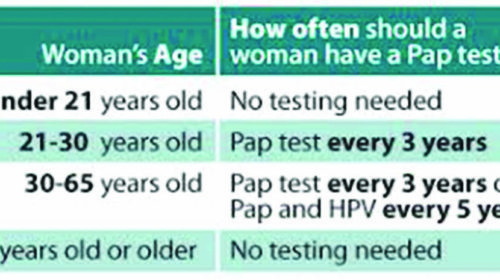
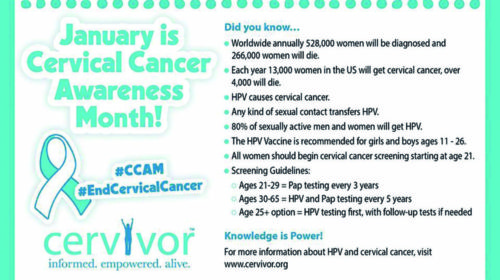
Screening
Screening aims to detect precancerous changes, which, if not treated, may lead to cancer. Women who are found to have abnormalities on screening need follow-up, diagnosis and treatment, in order to prevent the development of cancer or to treat cancer at an early stage.
WHO has reviewed the evidence regarding the possible modalities to screen for cervical cancer and has concluded that:
• screening should be performed at least once for every woman in the target age group (30-49 years) when it is most beneficial;
• HPV testing, cytology and visual inspection with acetic acid (VIA) are all recommended screening tests;
• cryotherapy or loop electrosurgical excision procedure (LEEP) can provide effective and appropriate treatment for the majority of women who screen positive for cervical pre-cancer;
• “screen-and-treat” and “screen, diagnose and treat” are both valuable approaches.
Regardless of the approach used, the key to an effective programme is to reach the largest proportion of women at risk with quality screening and treatment. Organized screening programmes designed to reach most women at risk are preferable to opportunistic screening.
Comprehensive approach to cervical cancer
WHO recommends a comprehensive approach to cervical cancer prevention and control that includes multi-disciplinary interventions across the life course. Community education, social mobilization, vaccination, screening, treatment and palliative care are needed to improve cervical cancer control. Almost all of cervical cancer deaths could be avoided if known effective interventions were available to all women and implemented, including immunizing adolescent girls against human papilloma virus (HPV) and cervical screening and treatment of pre-cancerous lesions.
To build on what exists and enhance progress, 7 UN agencies under the United Nations Task Force on NCDs have established a Joint Programme to prevent and control cervical cancer to provide global leadership and technical assistance to support governments and the partners build and sustain programmes.
Human Papillomavirus (HPV)
Human papillomavirus (HPV) is the most common viral infection of the reproductive tract. Most sexually active women and men will be infected at some point in their lives and some may be repeatedly infected.
The peak time for acquiring infection for both women and men is shortly after becoming sexually active. HPV is sexually transmitted, but penetrative sex is not required for transmission. Skin-to-skin genital contact is a well-recognized mode of transmission.
There are many types of HPV, and many do not cause problems. HPV infections usually clear up without any intervention within a few months after acquisition, and about 90% clear within 2 years. A small proportion of
infections with certain types of HPV can persist and progress to cancer.
Cervical cancer is by far the most common HPV-related disease. Nearly all cases of cervical cancer can be attributable to HPV infection.
Though data on anogenital cancers other than cancer of the cervix are limited, there is an increasing body of evidence linking HPV with cancers of the anus, vulva, vagina, and penis. Although these cancers are less frequent than cancer of the cervix, their association with HPV make them potentially preventable using similar primary prevention strategies as those for cervical cancer.
Non-cancer causing types of HPV (especially types 6 and 11) can cause genital warts and respiratory papillomatosis (a disease in which tumours grow in the air passages leading from the nose and mouth into the lungs). Although these conditions very rarely result in death, they may cause significant occurrence of disease. Genital warts are very common and highly infectious. (World Health Organisation)



